Delmarva Community Birth Stories: The Birth of Jude Thomas
/We've started something here! Our community is contacting us left and right and asking if they can share their stories. Ummmm.... YES! This was such a special birth for me. Although now that I'm thinking about it, they're all so special. Enjoy reading the story of the birth of baby Jude, written by his reflective and talented mother, Alaina.
Xo, Maria
“If He can hold the world He can hold this moment.”
Words from a favorite song at the time spoke to me months leading up to the conception of my fourth child and stuck with me through my pregnancy and birth. My husband and I decided to add on to our family during a time when many likely questioned “what are they thinking having a baby right now?” We chose not to put our lives on hold and move forward, because God’s plan is never our own. I was in tune with my body’s natural rhythm, experienced in sympto-thermal charting, and was prepared to make it happen. I wasn’t prepared for the struggle of conceiving this baby. Being the fourth child, I assumed I would conceive quickly like my others. My “struggle” seems relative because it can in no way compare to what others have gone through, including those close to me. Nonetheless, it was a difficult time of confusion, sadness, and anger. I had this idea in my head of what was to come and a timeline prepared in my head, as is my usual style. As with most things, my timeline fell to the wayside and baby #4 was finally conceived in March 2016.
The birth of my fourth child was a culmination of my previous births and everything I had learned. It was an experience that allowed to me to come full circle and to feel I had actually conquered what I knew I did NOT want the birth to be. To accurately describe this birth, I need to go back to the beginning. The birth of my first child was rather traumatic for me, so my goal with the subsequent births was basically anything to avoid a repeat. My daughter suffered a significant trauma to her neck due to shoulder dystocia and I was not in much better shape. With my second daughter I chose a route that I thought I was “supposed” to go. I chose to be induced a second time and got an epidural immediately. My mindset was if I don’t feel anything maybe it won’t happen again. It wasn’t until my third child that I realized what I experienced the first time was not “normal.” I had finally figured out that the way I thought birth was “supposed” to be was not at all accurate. I had learned that the trauma to me and my first daughter could have been avoided. I became more in tune to natural births, familiarized myself more with the trauma and came to learn so many things I had no idea about. With the birth of my third daughter I set out to have a completely different birth. I would not be induced and it would be a natural birth free from intervention. This baby would not have a shoulder dystocia and get stuck! Well, she did get stuck and I did receive pitocin after hitting that magical time clock after my water had broke before active labor began. Despite it not going exactly how I had planned, it was a major step towards a better birth experience with a different provider and different location. With my fourth I read and re-read countless books and familiarized myself even more with shoulder dystocia, determined to beat the odds that were stacked against me. I watched videos constantly of peaceful births, determined to have some quiet, introspective birthing experience. I actually wrote down a birth plan instead of just having ideas in my head. I practiced different exercises and positioning to avoid a possible repeat shoulder dystocia. I visited the chiropractor often, despite all of my midwife providers not acknowledging any correlation to adjustments, baby’s positioning, and shoulder dystocia. I had my plan in place. It would be perfect and peaceful and since it was my fourth it would be quick (HA!)
I knew at the beginning of this pregnancy that I wanted to hire a doula. I would be faced with many challenges and likely opposition given the extremely high risk of a third shoulder dystocia. Also, my babies were getting progressively bigger and having a cesarean was something I wanted desperately to avoid. I needed another person in my corner, someone to validate my decisions and not make me feel weak or feel strong-armed into something I was against. With all of my births I have always had my husband, mother, and mother in law present. To some this is a lot of people, but each had a very specific role that didn’t quite match up with what I would need from a doula. I needed my mother’s presence because she’s my mother. I think my first birth really terrified her so she generally took a back seat and waited patiently, offering support towards the end just enough to let me know she was there. This was what I needed from her. My husband offered physical support when I needed it, a hand to squeeze, and words of encouragement. I needed his presence more than anyone because he’s always been my rock and makes me feel stronger. But, he’s not so comfortable with birthing and always felt too out of his element to really learn more. I was comfortable with his feelings and did not pressure him into doing things he wasn’t comfortable doing. My mother in law, which is surprising to some, was the person that truly took an active role. In fact, she was a little offended that I would hire someone to take over what she thought of as her role. Okay, she was a lot offended. She has attended 12 of the 14 births of her grandchildren. She was with me for my previous three births. She was the one to coach me in my breathing and pushing. She was a calm presence, but also fierce. She has a strong personality, one that I knew would be confident in standing to protect me. At the same time, she generally sides with the typical medical stance and recommendations which I felt may not quite suit my stance with this particular birth. My births thus far had been far from ordinary and uneventful, which was something she was not accustomed to. So I hired my doula Maria, someone to share my birthing thoughts and plan and wouldn’t necessarily side with the medical professionals unless myself or the baby were in true danger. It was difficult balancing the roles of the doula and my mother in law “doula,” but I feel like it worked for me at least.
I had my team ready and I was ready. I chose to see the midwives in Easton for a second time and give birth at their hospital again. Despite the many changes I heard had taken place locally, the memories and sour taste in my mouth from the previous births were still there. I knew what to expect in Easton and felt my chances of having a midwife of a similar mindset was greater. I met with a few different midwives before I finally had an appointment to meet with one that I just knew would be of the same mind and be supportive of this birth, despite the risks. She had a wonderful reputation and I was hopeful. When I met her one of the first things she discussed was a scheduled cesarean and advised me to consider that route given my high risk of repeat dystocia. I was devastated. How could this be? None of the others had advised this and I thought for sure this woman would be the one to absolutely be in my corner. After leaving the office I immediately called Maria. I weighed my options of changing providers to Salisbury mid way through the pregnancy or continuing with what I felt was questionable support of the Easton midwives. I felt dismayed and defeated but chose to stick it out, feeling that in the end I at least had the support of my team. We would watch the baby’s size closely and revisit this later on if the baby seemed extremely large. In the weeks towards the end of the pregnancy I became much more aware of baby’s position. I could feel even the slightest angle of the head being not quite centered. I saw the chiropractor nearly every week and on a Friday, 2 days before the 41 week mark I noticed another shift in the baby’s head more to the side. Coincidentally the same side my others were stuck on. After an adjustment she used the rebozo on me to “shake the apples,” a technique among many I had read about and practically memorized on a website about spinning babies. I felt baby move and shift. At this time most would be growing impatient, but all of my children were born after the 41 week mark so I was prepared for that day to come and go. It was in the early hours the morning after, around 3 AM on Saturday December 17th, that my water broke. As I did with my last child I tried to convince myself I just didn’t make it to the toilet fast enough. At 3 AM that seems totally logical, right? So I used the bathroom, got back in bed and shortly after got the urge to pee again, partially feeling like I was actually peeing but mostly just gushing amniotic fluid. And that went on for the rest of the morning until my children woke us up. I told my husband, “I’m pretty sure my water broke last night.” He casually asked if we needed to go to the hospital to which I respond no, because I wasn’t having any contractions. I called Maria later that morning and told her the same, that I thought my water had broke but I may have just been peeing but as I said it out loud to someone who’s way more familiar with births than me I realized just how ridiculous I was being. Of course my water had broke, I just didn’t want to acknowledge that this birth was beginning the exact same way as my last. This birth was supposed to be different! My water was supposed to break and labor would actually begin and I would barely make it to the hospital before I had my baby, or maybe even have my baby on the hour and a half drive. HA! I walked around the house, bounced and rolled on my birthing ball, and listened to my husband blare on repeat “Hey Jude.” After three girls, we were hoping for a boy. I guess playing the song on repeat was one last ditch effort. I rested at times but mostly went about the normal day taking care of the kids having intermittent contractions of little intensity. We had an ice storm the evening before and the Vienna bridge was closed, so even if I wanted to go to the hospital I couldn’t have. We decided later in the afternoon after the bridge had reopened to head to the hospital. Even though there was really no established pattern to my contractions we didn’t want to risk the roads freezing again that night.
When we arrived at the hospital my contractions were still not regular and the ones I was having were not strong at all. Déjà vu. We walked, laid, bounced, massaged, prayed, and waited. It was later that evening that the midwife informed me that the person on the next shift was an OB, not a midwife. It was at this time I felt like I spiraled into fear. I felt like with an OB present for this birth I was for sure going to have a cesarean. Also, my water had broke and that time clock I was on with the last birth was slowly ticking away again. Though I didn’t acknowledge this time frame myself, I knew it would become an issue with the providers. So I called Maria to come to my corner and mentally prepared as much as I could for a fight with this OB. My mind was quickly put at ease when my new nurse came in and it was the one I had and loved with the last birth, Stephanie. She was such a calming presence and in that moment when my baby was stuck she calmed my fears and managed to quickly get me into a position to perform the McRoberts maneuver all while keeping me from freaking out and continuing to coach me through breathing and pushing. She was amazing and with her I again felt confident that this could finally be the intervention free birth I was hoping for. Another person on my team! Maria arrived to probably the calmest and most uneventful birth. She suggested side lying with the peanut ball which is when the contractions began getting stronger and developing more of a pattern. I knew that given the history of shoulder dystocia the best position I should birth in was on all fours. I prepared myself by first getting on my knees and then laying against the back of the bed. I remember laying my head down between contractions and falling into the strangest sleep/awake cycle for brief moments. I could actually hear myself snoring and I was aware of voices around me, but I didn’t really care what they were saying. I would quickly be awakened by another contraction and eventually felt the urge to start pushing. Pushing in that position against the back of the bed just came naturally to me. It was where I wanted to be and could easily sway from side to side. I labored and pushed like that for what felt like an eternity, with Maria applying the most wonderful counter pressure.
Eventually my knees became weak and I needed to try something different. The nurse brought in the squat bar. The thought of using this never entered my mind as part of my birth plan. I lay on my back between contractions and begged for a break. Like if someone could just press pause for an hour so I could rest I would be good to go. When each contraction began everyone would help hoist me up over the bar. The uneven bars were my favorite event as a young gymnast, but something tells me I probably looked a little less graceful with this bar! With the bar under my armpits, I held myself up and pushed through each contraction.
I reached a point of sheer exhaustion and couldn’t hold myself up. I resorted to lying on my back, even through contractions, which is exactly where I didn’t want to be starting out. Lying on your back is the worst position for a potential shoulder dystocia. I felt like I was failing giving in to this position, but looking back it was where my body needed me to be. It was at this time that the OB checked me and noticed I had a “cervical lip,” a swollen portion of my cervix. The baby’s head was pushing against this lip causing it to swell, further preventing baby from coming out. She suggested Benadryl to help reduce the swelling and in order for that to work I had to stop pushing. It was at this time she and the nurse also brought up pain medication to allow me get the rest I needed and to assist in refraining from pushing. I refused, then quickly said yes to IV meds, then quickly said yes to an epidural, and in my mind I was thinking “just cut me open” but thankfully I didn’t voice that one out loud. I was utterly defeated. Everything I did not want I was allowing to happen. In that moment where you have no idea where you are at in birth, how much longer it will be, and what exactly is happening your mind can wander in so many different directions. And oh how my mind strayed.
“If He can hold the world He can hold this moment.”
The Benadryl was administered and a bolus began in preparation for an epidural. This was by far the hardest part of the birth, lying there and having to breathe through a contraction without pushing. Is this even possible? Apparently it is but it wasn’t an easy pause button like I had hoped for. This was Maria’s shining moment. Though she was fully present, helpful, and supportive throughout the entire time, this was when I needed her most. She helped me to do quick breathing through each contraction. I’m pretty sure I may have broken a few of her fingers and melted her face with my horrendous breath, but she continued to breathe right along with me, right in my face to keep me focused and it worked. It was amazing, and wonderful, and horrible at the same time.
“If He can hold the world He can hold this moment.”
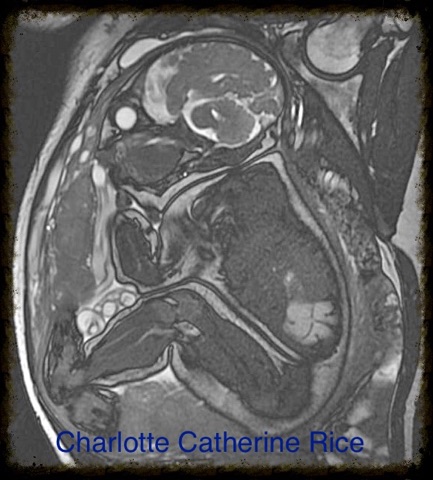
About 20 minutes after the Benadryl (I’m relying on other’s timeline here because my concept of time had escaped me long, long ago) I couldn’t breathe through the contractions any longer. I would start the quick breathing and would find myself pushing in the midst. There was no holding it back any longer. I was nowhere close to being ready for the epidural I had agreed to, but this was happening, the baby was coming and I was relieved that I wouldn’t be getting that epidural after all. The nurse or OB, I can’t remember because my eyes were closed, told me to stop pushing and I replied, or likely screamed I can’t, I HAVE to push. The nurse checked me and immediately gave me the ok, as if she could have stopped me anyway. The swelling was gone. I wasn’t prepared to feel so nauseous at this time though. After each contraction and pushing I would get a wave come over me and feel it rise in my throat but nothing ever came. Then I felt the “ring of fire” which was amazing. I’m sure no one describes it as such, but it was amazing to finally feel something that I knew and understood. It was something familiar and a kind of measure of progress and timing. I knew what it meant, where I was in the labor process, and I knew that my baby was finally coming. I don’t have a concept of how long I pushed partially because I was so exhausted, but also because I didn’t really care to know. I didn’t want to hold myself to anyone else’s standards nor have unrealistic expectations based on others experiences. I just wanted to push my baby out without getting stuck. And on December 18th, 2016 at 7:49 am I did! And not only did this baby not get stuck, but it was a BOY! A gigantic 8 pound 8 ounce baby boy; the largest of my babies and not even close to the predicted weight at the ultrasound just a few days prior. The wave of excitement and disbelief was so overwhelming that when they laid him on me I did not notice his coloring. He was on my chest briefly when they brought up the clamp and scissors to cut his umbilical cord and I immediately said “no no no.” My birth plan had included delayed cord clamping, something I had not done with my others but really wanted to with this one. The OB simply said “no, I have to.” I had no idea what was happening, but knew something was not right. I didn’t recall his heart rate changing at any point in time, but I quickly realized there were no sounds coming from my baby. Maria held my hand and comforted me telling me “he needs help,” a vague yet comforting response. I lay there, attempting to watch but being fully blocked, waiting, and praying. I carefully watched my husband as he stood next to our son, trying to read his face for some kind of clue as to what was happening.
“If He can hold the world He can hold this moment.”
And then our baby cried and I saw the emotional relief wash over my husband and I could breathe again.
This birth was anything but peaceful and introspective. It was not quiet, it was not quick, and it was far from what I had envisioned. Yet it was everything for me. There were hiccups and struggles, exhaustion and fear, but so much joy and hope in the process. I felt like I had conquered the odds that weighed so heavily against me. I had proved not only to myself, but to everyone around me (and hopefully some nay-saying medical professionals) that my gut intuition and the knowledge I gained from my shoulder dystocia research was all valid. The empowerment I wanted and needed didn’t have to come from a beautiful, peaceful birth that I had envisioned. This was enough.
After 15 years together, 10 years of marriage and 3 beautiful little girls, God finally gave us Jude. We had chosen the name Jude years ago as a nod to the Beatles and our love of all things 60’s. As our lives took a drastic turn from the path we had chosen, the name Jude came to take on a very different meaning in our lives. There is not a day in our lives that God has not already seen and though I never could have imagined the events that took place, God knew. Saint Jude calls us to be faithful and persevere under difficult circumstances, giving hope to the hopeless and despairing. God has heard our prayers and blessed us with Jude during a time in our lives when we were in absolute despair. He blessed us with Jude when I was feeling completely hopeless during labor, wanting to hit the pause button and take a break, then crying for it to just be over. He blessed us with Jude as we prayed for him to begin breathing. Jude is our sign of hope that things will be okay, a reminder to remain faithful. This may not be the road we have chosen, just as it was not the birth I had fully envisioned, but I know that God is with us on this journey as He was on December 18th.