The Birth of Eden
/Local mom Amanda retells the story of the birth of her second child, Eden. We're sharing this story on October 15, Pregnancy & Infant Loss Awareness Day. Eden's story is powerful, real, raw, and beautifully touching. I hope you can find some time in your day to remember baby Eden and send some good thoughts and prayers to Amanda and her family.
I’ll never forget the moment I found out I was pregnant with our second child. I had gone in for my annual gyno appointment, expecting to discuss birth control options with my provider because our daughter was 7 months old and I was finally feeling human again. To my surprise, my bloodwork came back positive. How could I be pregnant? Ok, I knew how I could be pregnant, but I was exclusively breastfeeding. Don’t the old wives say you can’t get pregnant while nursing? Aren’t the old wives educated medical professionals that bar out all acts of God with the collective wisdom of the ages? After informing my husband (and subsequently reviving him), I sat down to sort through my feelings. Fear and an overwhelming worry of how we would provide for two kids on one income and how I would mother two children under two all wrapped up in the promise of an even greater sleep deficit crept in first. I did what any overwhelmed mother would do in this situation-- feed the child snacks and pray I make it to bedtime. After some ice cream and the metaphorical “bedtime”, hope arrived. Excitement at the promise of a new life and all the potential love and laughter that would ensue filled my heart. I would just embrace the chaos, and take it one day at a time, cherishing the small things.
A few months, a handful of doctor appointments, and one sonogram later, we were ready to announce. It was December, and now that we had sonogram photos, we decided to do a Christmas themed announcement. Our daughter held a stocking that said “Big sister” and a photo of our newest bundle to be. The congratulations poured in over the next few hours. Here we were, about to be a family of four. I still wasn’t sure totally how to feel.
Three days later, on 12/13/14 I began to see spotting. Immediate dread filled my heart. I knew that blood, no matter how minute, was never exactly a good thing. We called the doctor, but of course it was the weekend so I had to wait for a call back. That was the longest 20 minutes I’ve ever experienced. Again, my thoughts wandered to “How?” This baby was perfect 72 hours ago during the sonogram. Perfect development, strong heart beat. How could it have ended so suddenly? The on call physician told me that there was really nothing that could be done at this point, that my body was “taking nature’s path.” They said only to come to the hospital if I was experiencing hemorrhaging, and that it was probably best to just ride it out at home because my fetus was 6 weeks short of being viable. They gave me no advice on what to expect next, so I tried to google without being sucked down the web-based medicine rabbit hole.
After laying down in bed, I tried to come to some sort of peace with what was happening. Spoiler alert: I’m still trying to come to terms with it, 3 years later. As the bleeding increased, I migrated to the only place I felt I could be, the bathroom. It was night, and I couldn’t bring myself to turn on the light to see what was happening. I knew when it was over, and I sat there pondering if I could bring myself to reach down into the toilet bowl and hold my child. I couldn’t. I felt like a terrible mother. Not only could by body not provide and protect this baby, but I couldn’t muster up the courage to hold him or her before having to just dispose of him or her because they were not “viable”. I didn’t deserve this angel, and that’s why the opportunity was taken away. My mind was a dark place thinking that somehow this was my fault.
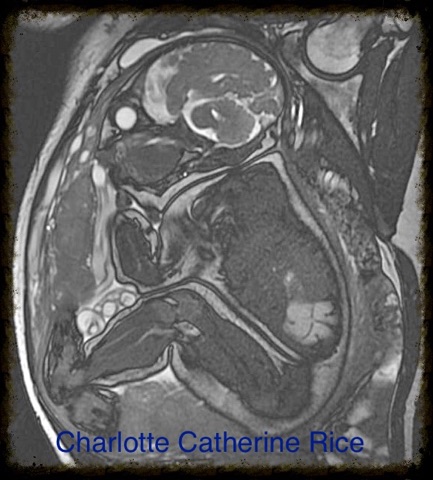
I went to the doctor the following day, where a sonogram showed my empty womb. While the doctor tried to be sympathetic, I saw what she entered in my chart. “Complete abortion” hit me like a brick wall. I always felt like abortion was something you chose. I did not choose this. I would not in a million years choose this. There had to be a better term. When it’s referred to it as a miscarriage, I feel like that defines the death of the child but not the birth. The process IS birth. I only really noticed that’s what it was because I had already had a vaginal delivery. The waves of contractions, the overwhelming instant relief as soon as the baby is born are exactly the same. I can’t speak on the variations of the degrees of pain, as it may be less for someone who experienced loss earlier in their pregnancy. I was 18 weeks at the time but this was birth just the same.
Six months later, there were two pink lines. Nine months after that, on Valentine’s Day, our rainbow baby boy was born [read that birth story here]. Full of love and laughter, escorted earthside by his angel sibling. It was a healing moment for me physically because I spent my entire pregnancy expecting to lose him too. The anxiety was a constant burden, and that was an unexpected side effect from this whole experience.
I lost a child, but I found a village. People sent their condolences, and hidden in quite a few more of those condolences than I ever expected were privately messaged stories of their own losses. Because of the stigma, especially for older generations, I never knew how many mothers were in this horribly cruel club. Losing your child is a pain I wouldn’t even wish upon my worst enemy. Part of the healing for me was sharing in this web of collective grief. I was not alone. So many others understood my pain. They felt the crushing guilt that I was feeling. “Maybe if I had been better, healthier, more vigilant, etc.” was the general consensus, even though we all know we couldn’t have prevented it. You can’t keep the darkness from creeping in, but it’s comforting knowing that others came before you to help show you the light.
The village wasn’t all that came from this. I learned how my husband grieves. During the loss, he was distant. He kept saying things to assure me that I was fine and was trying to be optimistic. We never spoke much about it. A few months after, a teacher from my high school, who is now a genetic counselor, had posted a link to a research survey about how couples deal with pregnancy loss. There was a questionnaire to be filled out separately by both the mother and the father. This survey is finally what allowed him to open up and express his grief. He tried to be the strong one for me, and I mistook his distance and nonchalance for apathy. Our marriage grew from this new understanding, and I was able to tell him that I had silently named our baby. Seeking out something gender neutral as my loss occurred two weeks before the anatomy scan, I had decided upon calling him or her Eden. My paradise, lost.
I learned a lot about myself as well. I learned to be patient with my children because some are not so lucky. I must be more empathetic to strangers, as they are the only ones who know what they are carrying around today. I cannot be jealous of those that haven’t felt this pain because for some unknown reason I was chosen to shoulder this load and I will do it to prevent their pain. Most importantly, I learned how to be kinder to myself. There’s good days and bad days, days where I fail to notice the absence of our other child and days where the soul shattering emptiness feels like it will swallow me whole. On days like the latter, I must take time to grieve. One hearty, ugly cry at a time, I hope to be slowly reassembled. The memories I make with the children I get to keep here on earth with me will fill the cracks and become the glue that holds me together. Until we meet again, my angel baby, Eden.